![]()
![]()
Stroke recovery begins with understanding what a stroke is and how it disrupts brain function. A stroke occurs when blood flow to a part of the brain is interrupted or reduced, depriving brain tissue of oxygen and nutrients. Within minutes, brain cells begin to die. Ischemic strokes, caused by blood clots blocking arteries, are the most common type. Hemorrhagic strokes, caused by ruptured vessels, are less common but often more severe.
Each type impacts the brain differently, and this shapes the recovery journey. Knowing the exact nature of the stroke helps guide appropriate treatment and rehabilitation strategies. It also gives patients and families realistic expectations and helps in forming a focused recovery plan. Recognizing stroke symptoms sudden weakness, facial droop, confusion, or vision loss, can speed up emergency care and minimize damage. When you grasp the biology of a stroke and its effect on the brain, you’re in a better position to make informed decisions throughout the recovery process.
Understanding how a stroke affects specific areas of the brain explains why some people struggle with speech, while others face mobility challenges. A stroke on the left side of the brain might cause right-side body weakness and language issues, while a right-brain stroke often leads to spatial awareness problems and left-side weakness.
Stroke recovery isn’t just about regaining strength it’s about helping the brain rebuild pathways that were interrupted. This can involve therapy to retrain speech, occupational tasks, or relearn how to walk. It all begins with a clear picture of the damage done and the specific functions that were compromised. The more accurately the stroke is diagnosed and understood, the more effective the recovery interventions can be.
Accurate diagnosis also helps prevent future strokes. Imaging tools like CT scans and MRIs are critical for identifying the cause and extent of damage. Blood tests and heart monitoring can uncover underlying conditions like atrial fibrillation or high cholesterol. This level of detail doesn’t just inform immediate care, it becomes a guide for lifelong prevention. Stroke recovery doesn’t end when someone leaves the hospital. It’s a continuous process rooted in knowledge, consistency, and well-informed treatment decisions.
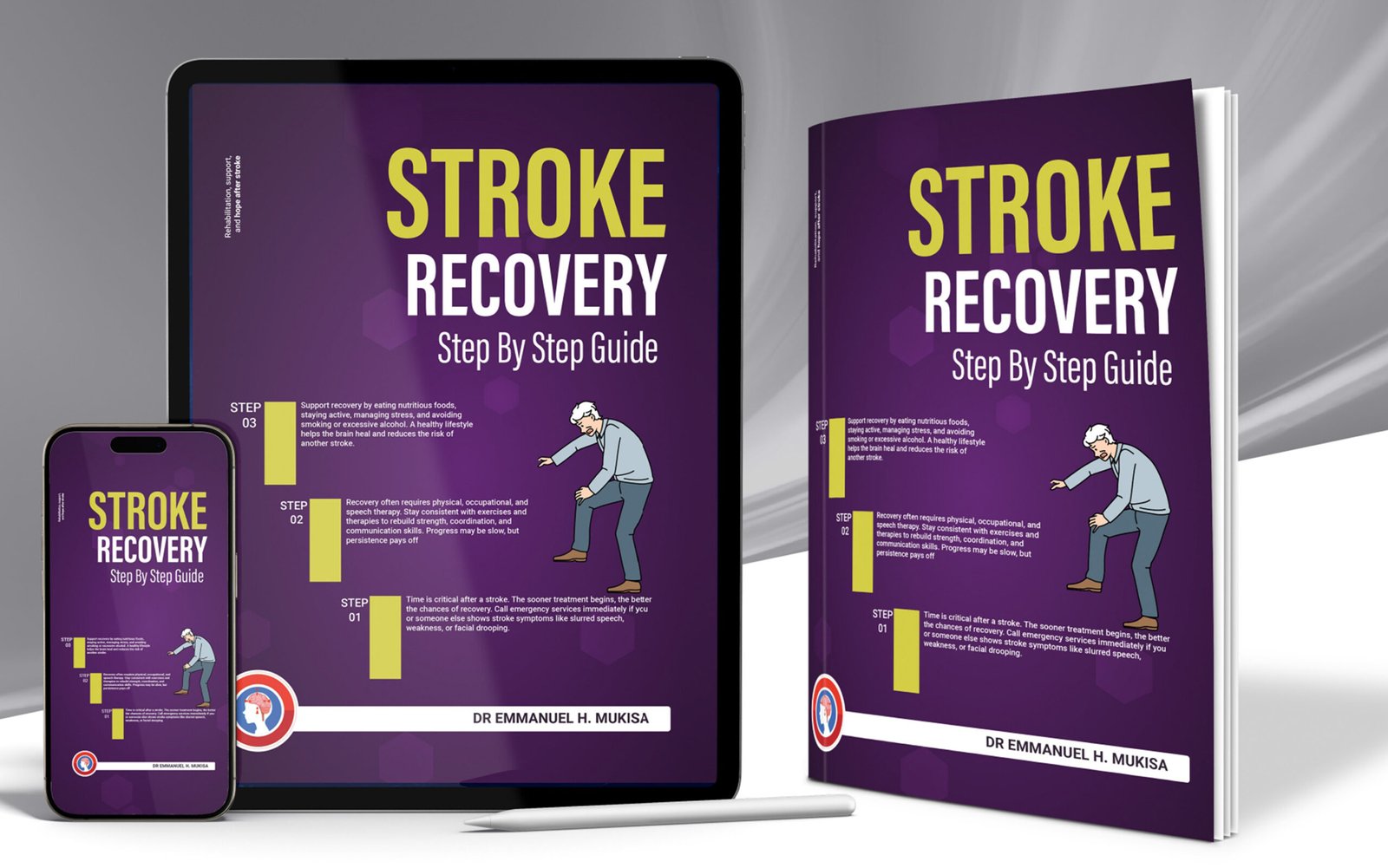
Every minute counts after a stroke. Immediate medical attention within the first few hours determines whether damage can be reversed or contained. In ischemic strokes, clot-busting drugs such as tPA must be administered within a narrow time window, usually within 4.5 hours of symptom onset. Missing that window can lead to irreversible damage. This makes it critical for family, friends, or even bystanders to recognize stroke symptoms early and act fast.
Emergency responders must be alerted immediately, and patients should be taken to stroke-ready hospitals equipped to deliver rapid treatment. Without this initial intervention, stroke recovery becomes more difficult and less complete.
Quick hospital assessment typically includes imaging to determine stroke type and severity. This shapes the initial treatment plan. Patients might receive medication, undergo a mechanical thrombectomy, or be monitored for complications such as bleeding or brain swelling. The speed and accuracy of this initial care often make the difference between temporary disability and long-term impairment.
It’s not just about survival, it’s about preserving brain function. Stroke recovery outcomes improve significantly when early intervention is done correctly and on time. Even after the immediate danger has passed, patients are closely watched for issues like blood pressure instability, breathing problems, or secondary strokes.
This monitoring phase is crucial. It allows doctors to adjust treatment, manage risks, and prepare patients for the next phase: recovery. Skipping or delaying these early medical steps can prolong disability, increase complications, and make rehabilitation harder. In stroke recovery, what happens first matters most.
The first 24 hours after a stroke are unpredictable. Patients may experience swelling in the brain, fluctuating consciousness, or sudden changes in blood pressure and heart rate. Medical teams focus on stabilizing vital signs and starting supportive treatments. Nutrition and hydration must be managed carefully, especially if the patient has trouble swallowing.
Respiratory support may be needed. These basic interventions set the stage for everything that follows. Stroke recovery depends on creating a stable platform early on. The neurological team evaluates consciousness, motor skills, reflexes, and cognitive function multiple times within the first day. This helps doctors assess the extent of brain damage and tailor a personalized treatment plan.
Some patients may be transferred to intensive care units, while others can stay in specialized stroke wards. Either way, observation during this period is intense. Any misstep, such as allowing dehydration or not managing blood pressure, can undo earlier progress. The body’s natural inflammatory response to a stroke must be controlled to avoid further injury.
Emotional reactions also emerge quickly after a stroke. Patients might feel scared, confused, angry, or frustrated, especially if speech or movement is impaired. The support they receive in those first few hours from both medical staff and family lays the groundwork for psychological recovery. Encouragement, clarity, and presence matter as much as medications or equipment. The first day is not just about surviving, it’s about building confidence that recovery is possible.
Without a plan, stroke recovery becomes guesswork. A strong recovery plan starts with a full assessment of physical, cognitive, and emotional needs. Doctors and therapists work together to determine which functions were lost and what level of independence is possible. This often includes physical therapy for mobility, speech therapy for communication, and occupational therapy for daily tasks.
Each element is tailored to the individual, and goals are realistic, specific, and time-bound. Recovery isn’t one-size-fits-all, and the plan must reflect that. Consistency is what makes a stroke recovery plan effective. Patients need daily routines that include therapy, medication, rest, and monitored activity. Skipping sessions or interrupting treatment disrupts brain healing.
The brain requires repetition to rebuild neural connections. This means practicing the same motion or skill many times a day, even if progress feels slow. A good plan builds these repetitions into daily life without overwhelming the patient. Family involvement, encouragement, and structure make all the difference.
Plans should also evolve as recovery progresses. What works in the hospital won’t always be right at home. Follow-up assessments help adjust therapy and medication, address setbacks, and introduce new strategies.
Stroke recovery takes months or even years, and the plan must adapt to new challenges. When a recovery plan is clear, flexible, and actively followed, patients regain function faster, stay motivated, and are less likely to suffer another stroke.
Mobility loss after stroke is common, but it doesn’t have to be permanent. Targeted therapy begins as soon as patients are stable, sometimes within 48 hours of the stroke. This early movement, known as mobilization, prevents muscle stiffness, pressure sores, and blood clots. It also stimulates brain recovery by encouraging the use of damaged neural pathways.
Even sitting up in bed, shifting weight, or moving limbs helps. Stroke recovery speeds up when the body is not left idle. Physical therapists focus on balance, walking, posture, and muscle control. Recovery exercises start small and build up gradually. Walking aids, parallel bars, or braces may be used early on. These tools support independence while the body relearns movement. Progress can feel slow, but consistency is everything.
Therapy sessions are structured, repetitive, and goal-focused. The aim is not just to move, but to move safely and efficiently. This lowers the risk of falls and helps patients return to daily life faster. As patients gain strength, exercises increase in complexity. Stair climbing, dressing, cooking, or simple outdoor walks may be reintroduced.
Emotional support during this phase is crucial. Many stroke survivors feel discouraged or fearful. Rebuilding physical strength also means restoring confidence and self-trust. Stroke recovery depends as much on mindset as muscle. With steady physical therapy, both can grow together.
Nutrition plays a direct role in stroke recovery. The right foods help rebuild damaged tissue, support brain function, and prevent another stroke. Many stroke survivors have trouble swallowing or a loss of appetite, which leads to poor nutrition. This makes early dietary intervention critical. Registered dietitians often step in to ensure patients get enough calories, protein, and nutrients.
Liquids, soft foods, or feeding tubes may be used short-term. The goal is to nourish the body without stressing it. Once swallowing improves, patients transition to regular food that supports recovery. A stroke recovery diet includes lean proteins, healthy fats, fruits, vegetables, and whole grains. It also avoids salt, sugar, and processed food. This reduces the risk of blood pressure spikes, diabetes, and cholesterol build-up, all of which increase stroke risk.
Hydration is also essential. Even mild dehydration can slow brain healing and cause fatigue or confusion. Every meal is an opportunity to heal faster and protect the brain. Nutrition education is part of long-term stroke recovery. Patients and families learn how to read food labels, plan meals, and avoid dietary traps. Cooking skills may need to be relearned or adapted. Lifestyle changes take effort, but they pay off. A healthy diet does more than repair damage; it empowers patients to take control of their future. Stroke recovery strengthens when nutrition becomes a daily habit, not a temporary fix.
